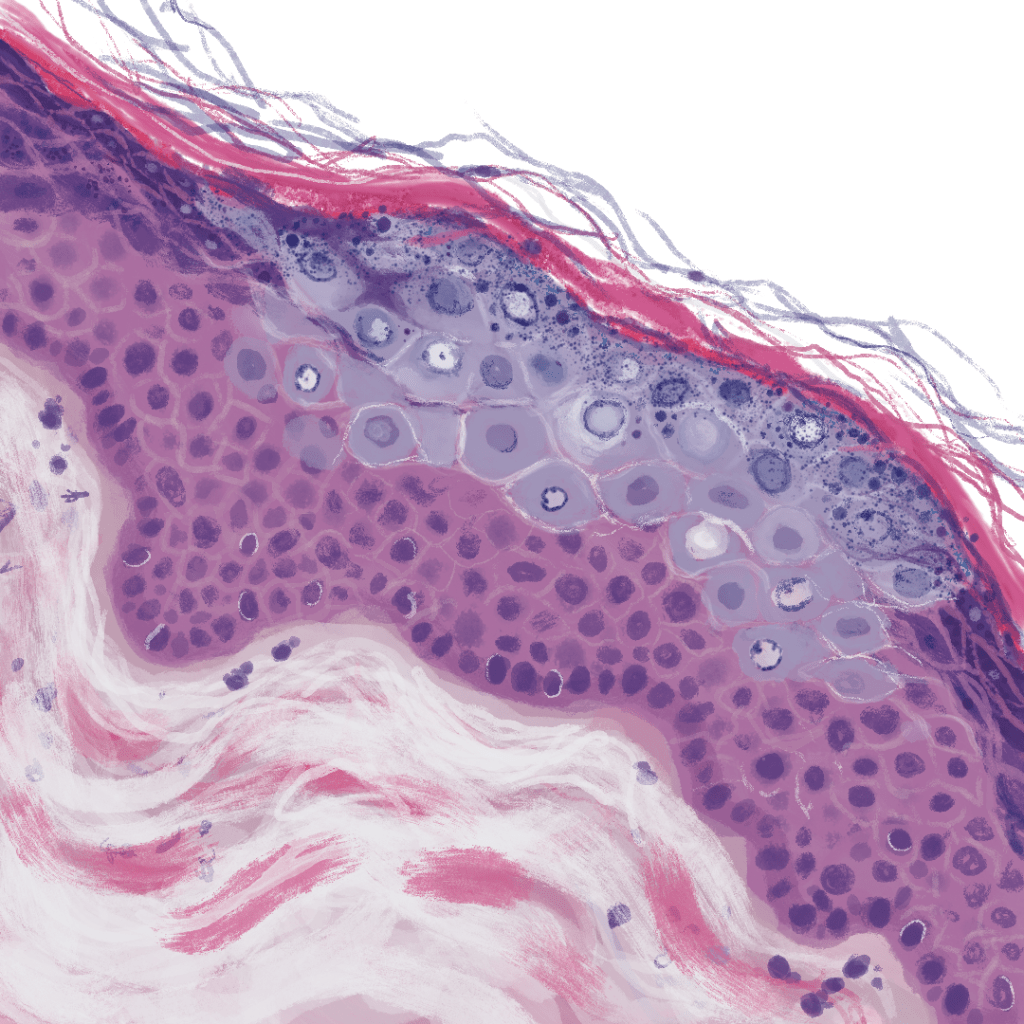
What you’ll notice first here is the color. EDV has a characteristic collection of unfortunate keratinocyte with blue-grey cytoplasm. Absolutely gorgeous… as the great Steve Irwin might say. Why I say “unfortunate” is because these cells are severely infected with HPV.
What types of HPV? So glad you asked. Classically, HPV types 5 and 8 are implicated in this condition, however others can be responsible. “And how am I going to remember this?” All you have to remember is that EDV is caused by HPV. Allow “E” and “H” to take on their respective numbers in the alphabet, which are 5, and 8. Pretty neat!
Now, most of the time this histopathologic finding is going to be incidental, a little easter egg in your BCC or SCC rule-out biopsy, which is what this drawing was based on. Within this context, most dermatopathologists won’t even mention the finding as it’s of no clinical significance.
Very, very rarely, the EDV itself can be the pathology. EDV is an autosomal recessive mutation in the EVER1 and EVER2 genes, which are thought to be responsible for intracellular zinc distribution. Warts grow in a severe and uncontrolled fashion to the extent that this disease was once referred to as “treeman syndrome” due to the bark-like appearance of the person’s skin. A handful of individual cases have been highlighted in recent history.
Aside from the inherited version, persons infected with HIV are susceptible to “acquired epidermodysplasia verruciformis,” in which individuals can get widespread wart involvement that, unfortunately, does not appear to receive with initiation of anti-retroviral therapy.
A common complication of both the inherited and acquired versions is advancement to squamous cell carcinoma.
Returning to the pathology, we recognize other characteristics that are commonly seen in HPV-related dermatopathology.
A pronounced granular layer.
Very large, chunky, keratohyalin granules, especially within infected cells.
Cleared out nuclei with funky, chunky chromatin.
Leave a comment